Innovaccer Launches AI-Powered Readmissions Management Solution to Help Health Systems Reduce Costs and Improve Care Transitions

Innovaccer has introduced a new AI-enabled Readmissions Management Solution aimed at helping healthcare providers reduce avoidable hospital readmissions, standardize transitional care, and improve resource utilization—particularly across Medicare, Medicaid, and uninsured populations.
The launch comes as hospitals prepare for increasing penalties under the Centers for Medicare & Medicaid Services (CMS) Hospital Readmissions Reduction Program (HRRP). In 2025, over 200 hospitals are projected to face penalties exceeding 1% of their Medicare revenue—translating to more than $1 million per institution in some cases.
Targeting Avoidable Readmissions Through Data and AI
The new offering integrates Innovaccer’s Data Activation Platform with predictive analytics, care management workflows, and AI-powered automation tools. The platform aims to identify patients at high risk of readmission and coordinate timely interventions that reduce preventable hospital stays and associated costs.
“Innovaccer is uniquely positioned to help health systems tackle avoidable readmissions, not just for compliance, but as a strategic lever for reducing cost and improving patient outcomes,” said Abhinav Shashank, Co-founder and CEO of Innovaccer. “Our solution brings together predictive analytics and AI-powered workflows that support timely, coordinated interventions.”
Growing Financial Pressure on Hospitals
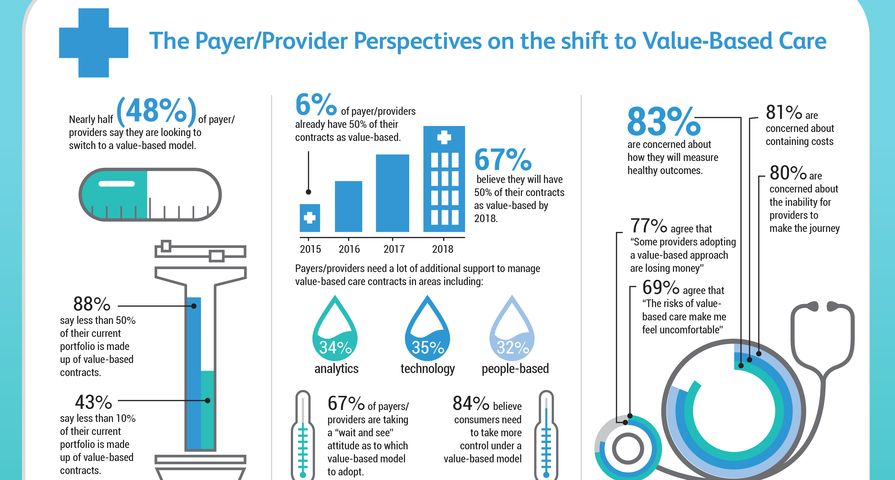
Avoidable readmissions not only affect reimbursement but also place a burden on hospital capacity, often occupying beds needed for higher-margin procedures. Hospitals with longer average stays, more Medicare patients, and higher volumes of chronic or complex cases are at increased risk. Uncompensated care costs, which already account for 2%–6% of operating expenses, are expected to rise—particularly in states affected by Medicaid spending reductions.
Key Features of Innovaccer’s Readmissions Management Solution
The platform combines data-driven insights with operational tools to support care teams in managing transitions and reducing readmission risk. Key features include:
- Predictive modeling: Identifies patients at high risk for readmission across Medicare, Medicaid, and uninsured populations.
- Care coordination tools: Out-of-the-box workflows tailored for transitional care management (TCM) and post-discharge follow-up.
- AI-powered agents: Includes tools like the Care Management Copilot and Pre-Call Coordinator Agent to streamline documentation and outreach.
- 360-degree patient and population views: Unifies clinical and claims data for more informed decision-making.
- Custom dashboards: Enables tracking of readmissions, outcomes, and performance metrics.
- Benchmarking intelligence: Utilizes VRDC data to help identify improvement opportunities.
- Targeted outreach: Automates communication with low-touch patients to reduce care manager workload.
Clinical and Operational Use Cases
According to Innovaccer, the platform supports reimbursement through TCM and primary care provider visits, reduces uncompensated care, and helps hospitals make more effective use of inpatient resources. The solution is built to support both value-based care models and fee-for-service environments.
“Innovaccer helped us prepare for MSSP participation by ensuring our Care Navigators have easy access to the right data and protocols to make timely and reliable clinical decisions,” said Dr. Mary Kim, Chief Medical Officer and Vice President of Population Health at Adventist HealthCare.
Availability and Integration Options
The solution is now available for existing customers, with additional capabilities in development. New users can integrate the platform as a full-stack solution or as a modular layer added to existing systems.
With mounting financial and operational pressures tied to readmission rates, Innovaccer’s latest offering is positioned to help healthcare organizations take a more proactive, data-informed approach to care transitions and system-wide efficiency.