CLARA Optics Enables Insurance Leader to Improve Medical Outcomes for Injured Workers
Western National Insurance have selected CLARA Optics, an AI-driven technology platform developed by CLARA Analytics (“CLARA”), to help improve medical outcomes for injured workers, increase efficiencies in workers’ compensation claims management, and ease administrative burdens on adjusters and nurse case managers (NCMs).
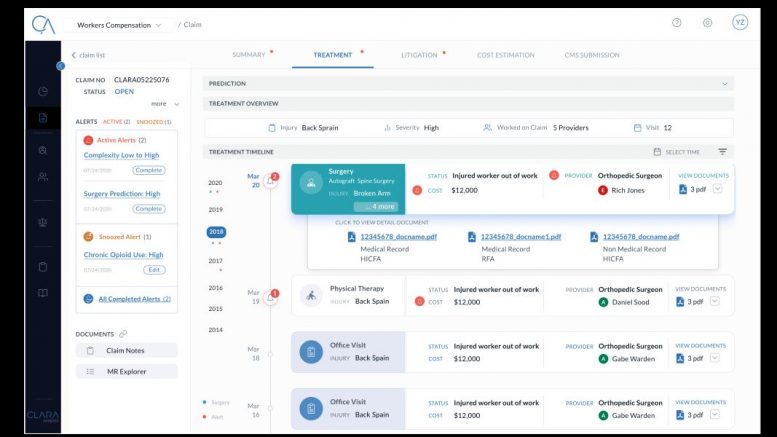
CLARA Optics automates medical records transcription, extracts and organizes important details about each case, and creates a claims-based medical record that highlights relevant information for claims management personnel. Optics constantly scans for new information, offering intelligent alerts whenever new case material becomes available. That empowers adjusters and NCMs to respond promptly and proactively as each case evolves. Advanced analytics empower claims managers to explore and discover relevant details that might otherwise have gone unnoticed.
“CLARA Optics is a game-changer for us,” said John Buckley, Senior Vice President of Claims at Western National Insurance. “Workers’ compensation claims management has always been a very tedious process, requiring adjusters to digest huge volumes of information, constantly monitor for changes, and make judgment calls based on their experience and intuition. CLARA’s technology provides our team with a powerful new tool that captures relevant details, highlights the most important information, and gives us a data-driven foundation for evaluating potential next steps. That makes our people even more effective in delivering top-quality service to injured workers.”
As the leading provider of artificial intelligence (AI) technology for commercial insurance claims optimization, CLARA offers a suite of complementary products that work alongside Optics. CLARA Treatment helps carriers determine which healthcare providers are most likely to produce positive patient outcomes; CLARA Triage spots potentially costly claims before they escalate; and CLARA Litigation assesses risk and helps carriers manage attorney performance.
CLARA’s award-winning AI platform is capable of analyzing both structured and unstructured data, performing contextual analysis using natural language processing (NLP), and generating predictive analytics to help claims managers make sound data-driven decisions. CLARA’s customers consistently achieve outstanding ROI, with some exceeding 500%.
“Western National Insurance is constantly seeking innovative ways to provide efficient and timely service for workers’ compensation claims,” said Heather H. Wilson, CEO of CLARA Analytics. “We’re thrilled that Western National has chosen CLARA to be their partner in that innovation. Together, we’re applying AI and machine learning to provide adjusters claims guidance from the hundreds of pages of medical records they receive daily.”
CLARA’s Optics module is priced on a per-page basis, allowing adjusters and NCMs to revisit case details as often as they like, without incurring additional costs for new reports. As additional information becomes available, pertinent case details are automatically captured and updated, giving claims management professionals vastly improved visibility into important changes as soon as they happen.