Zebra study reveals plans to mobilize urgent care teams, automate workflows, and regain control of supply chains
Zebra Technologies Corporation, an innovator with solutions and partners released the findings of its latest healthcare vision study. The “Smarter, More Connected Hospitals” global report reveals a stronger commitment to advanced technology tools as acute care providers strive to become more resilient and digitalize the patient journey.
Eighty-nine percent of executive decision-makers and 83% of clinicians surveyed agree real-time intelligence is essential for optimal patient care, and hospitals are increasingly investing in clinical mobility tools, real-time location systems (RTLS) and intelligent workflow solutions to support smarter, more connected workflows. However, more than two-thirds (67%) of hospital executives still don’t feel their organizations are investing enough to maximize staff efficiency and more must be done moving forward.
“The COVID-19 pandemic has tested the efficiency of both clinical and administrative workflows,” said Chris Sullivan, Global Healthcare Practice Lead, Zebra Technologies. “As a result, today’s healthcare leaders face the challenge of recalibrating technology systems to better support the needs of clinicians and patients.”
Need for Intelligent Workflow Automation
Approximately two-thirds of executives acknowledge physicians and caregivers are overextended during their shifts and spend too much time locating medical equipment and supplies. Over half report their administrative staff is equally overburdened and unable to complete their work during their shift. With people’s safety and well-being always the top priority, hospital executives are turning to technology to help combat fatigue, reduce errors caused by manual processes and workarounds, and refocus clinicians’ time on patients:
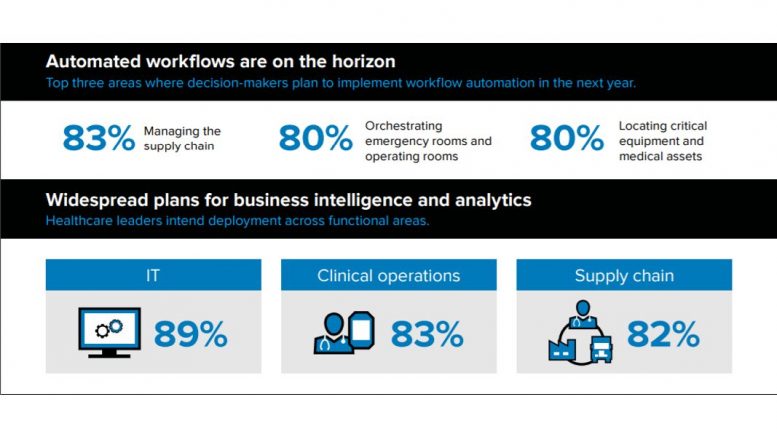
- Approximately 80% of executives plan to automate workflows in the next year to improve supply chain management, make it easier to locate critical equipment and medical assets, better orchestrate emergency rooms and operating rooms, and streamline staff scheduling.
- About three-quarters plan to use locationing technologies such as radio frequency identification (RFID) to better track equipment and specimens and improve patient flow and security. They are also turning to locationing solutions to create more dynamic workflows and improve staff efficiency, safety and compliance.
- Just as many executives say they will integrate visionary solutions like Internet of Things (IoT) sensors, prescriptive analytics, and artificial intelligence (AI) to help improve both inpatient and outpatient care as the opportunities for remote physician-to-patient and clinician-to-clinician consulting grow.
“Hospital staff must be able to identify, track, locate and monitor the condition of every patient, staff and asset. A mobile device alone can’t do that. That’s why we’re seeing rapid investment in locationing and automation solutions,” explains Sullivan. “It’s the technology that will work behind the scenes to improve front-line clinician workflows and the patient experience.”
Purpose-Built Mobility Solutions Drive Manageability
The majority of respondents (84%) believe the quality of patient care would improve if nurses, physicians and non-clinical healthcare workers had access to collaboration tools and the convenience of using their mobile devices to access healthcare applications.
This may come as a surprise considering that mobile technologies have been used in both clinical and non-clinical workflows for several years. By 2017, most bedside nurses, doctors and lab technicians were already using mobile devices, and adoption among pharmacy staff and intensive care unit nurses was on the rise. However, several acute care facilities were allowing staff to use their personal devices to connect to healthcare information systems and workflow applications at the time.
The approach to mobility is now changing. Nearly half (49%) of the surveyed executives now provide employees with hospital-owned devices intended for healthcare as more clinicians need durable and rugged devices, hospitals require more remote device management capabilities, and data security becomes a top priority. Those who have already adopted clinical mobility solutions are seeing the positive impact on the quality and cost of patient care with 8-in-ten citing an increase in medical workflow accuracy and precision as well as a reduction in preventable medical errors among other benefits.
All Technology Investments Tied to Workforce Transformation
Most hospital executives expect to have devices deployed across nearly all staff types in the next five years. However, the focus now is on nurses assigned to emergency departments, critical and intensive care units (ICU), and operating rooms as well as those responsible for IT, supply chain/inventory management and patient transport. This is a bit of a shift from 2017, when bedside nurses and facilities management staff were being prioritized for device deployments.
“Improving team communication is now a top goal of many hospitals, and executives are highly concerned about preventing the spread of infection and current staff burnout,” says Rikki Jennings, Chief Nursing Informatics Officer (CNIO), Zebra Technologies. “There is also a push to automate the orchestration of high traffic areas such as emergency rooms and operating rooms in the next year, which requires departmental staff to have mobile devices in hand.”
In addition, telehealth and remote patient tracking are rising on executives’ priority lists, both of which are poised to benefit ICU and emergency room staff, and forward-thinking leaders want to start the transition from manual, reactive processes to more responsive, predictive systems in the next few years.
As a result, most procurement and IT teams are now working to equip all staff with mobility solutions that enable them to access intelligent communications and locationing tools and take full advantage of automation solutions designed to streamline workflows and improve care delivery models. In fact, just as many doctors, pharmacists, radiologists and lab technicians are expected to have a device in hand in the next two years as emergency and critical care clinicians.
“More than ever, it is vitally important that all hospital functions work together as a cohesive ecosystem. That is only possible if they are plugged into the right information systems and one another,” adds Jennings. “Most of hospital’s transformation ambitions are either rooted in or dependent on mobile technology in some capacity. So, ensuring each staff member has a clinical device in hand is the first step to achieving a new standard of patient care and operational efficiency.”