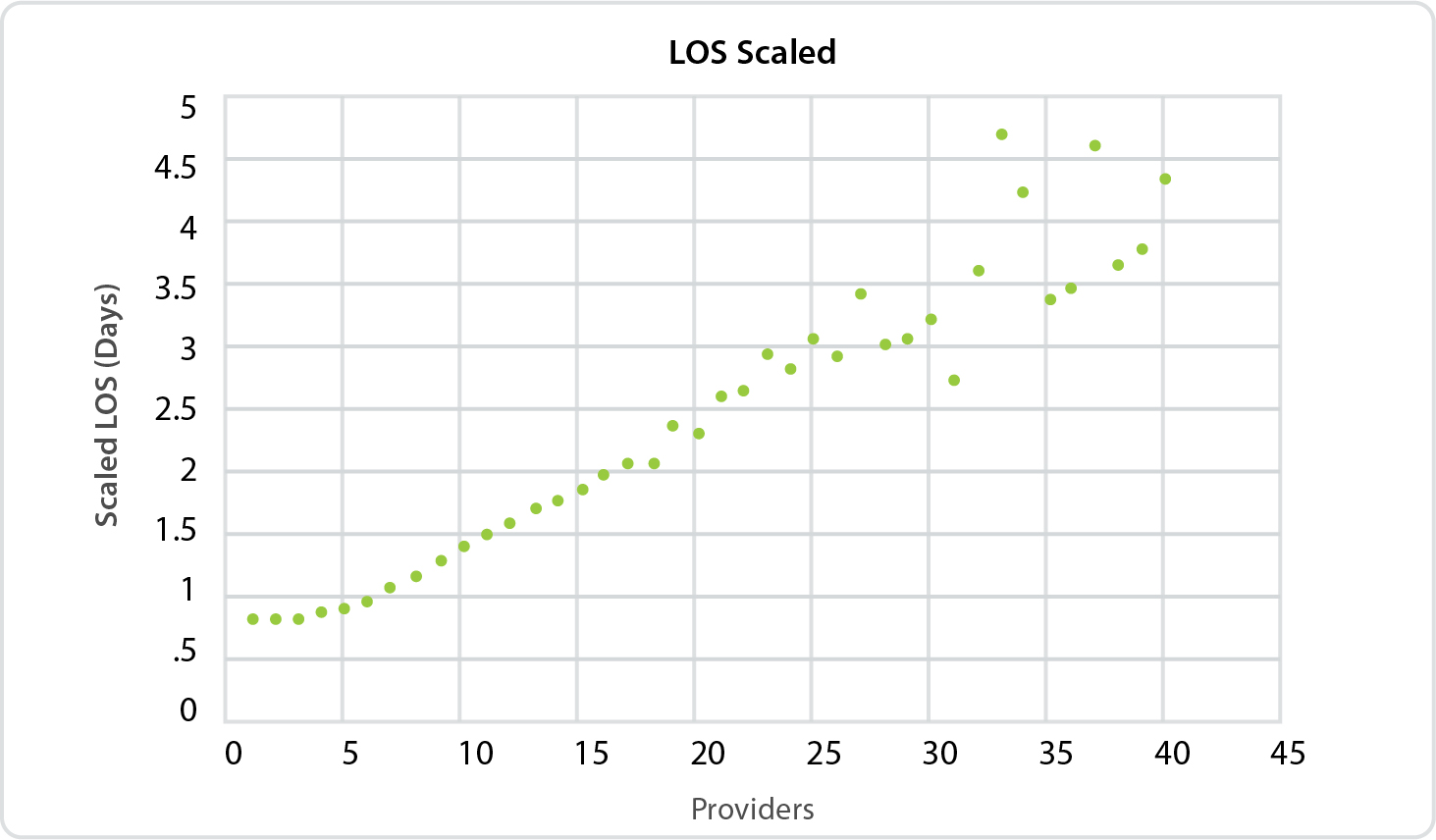
Every additional provider involved adds nearly an extra day in the hospital, on average
Patients may think that more providers involved in their treatment means more expertise that leads to better overall care. However, a new report by IllumiCare, a leader in point-of-care technology, is showing that having more providers significantly increases patients’ length of stay.
IllumiCare’s research focuses on the correlation between the number of actively involved providers (those who have written a medication/laboratory/
Once the patient’s stay passes three providers involved and three days in the hospital, each additional provider adds 0.58 days to the length of stay. With the national average for a hospital stay at 4.5 days, according to the Agency for Healthcare Research and Quality, fragmentation of specialties in the inpatient setting may be fostering inefficiencies.
As one of the top quality and financial metrics hospitals used to track performance, this increase in stay due to increasing handoffs and specialty consultations is not trivial. According to data compiled by the Kaiser Family Foundation, the U.S. average cost per hospital day is $2,424.
The Effect is Specialty-Independent
One important assumption the report refutes is the idea that one hospitalist handing off to another hospitalist is different than the one hospitalist consulting a cardiologist or a neurologist. The number of different specialties did not seem to matter. The analysis shows that even patients who saw only one or a small number of different specialties saw an increased length of stay. Each provider brings their own background, practice habits, preferences, etc. to the case. Also, there is often an imperfect information exchange from one provider to the next.
The Tendency to Consult Other Specialists Varies Widely
Given the correlation between the number of providers and length of stay, “over-consulting” may be a behavior to discourage. We found wide variation in hospitalist practice of consulting other specialists.
The report looks at hospitalists who wrote a medication/laboratory/
“This data is the perfect representation of the common saying, ‘Too many cooks in the kitchen,’ clearly demonstrating the challenges hospitals face in streamlining care. Executives are looking to get a better hold on provider behaviors that drive unnecessary cost and risk. Since medicine is not formulaic, it is difficult to manage each providers practice habits and tendencies, like the habit of consulting. Our goal is to shed more light on various provider habits that not only increase the cost of care, but also risks to the patient, and help executives and care teams be more judicious,” said G.T. LaBorde, CEO of IllumiCare.
To view the full report, visit https://www.illumicare.com/ereport-2/.