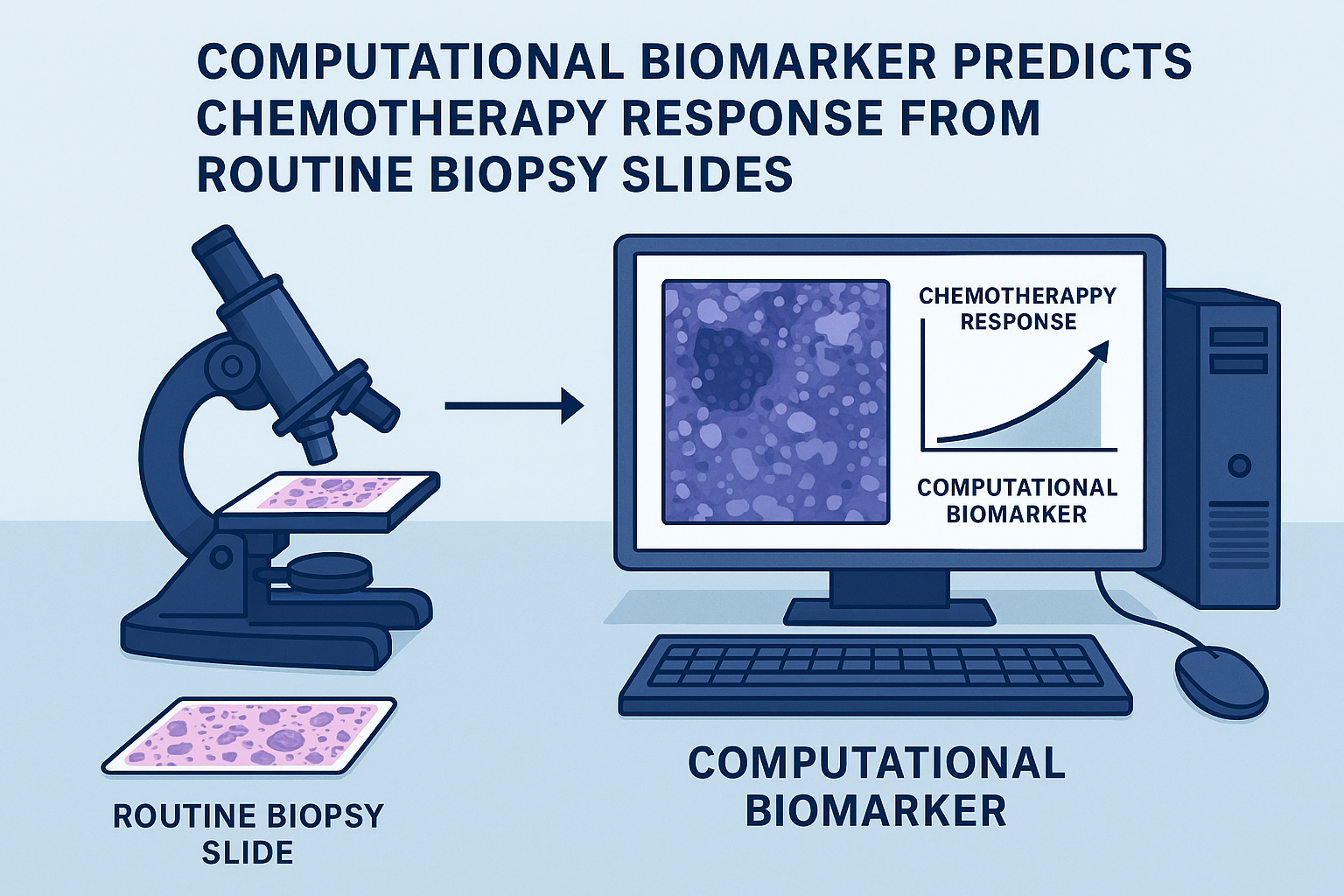
Computational Biomarker Predicts Chemotherapy Response from Routine Biopsy Images
Phase II TBCRC-030 Trial Demonstrates Image-Based Prediction of Residual Cancer Burden in Early-Stage TNBC
A recent analysis from the Translational Breast Cancer Research Consortium (TBCRC) 030 clinical trial has demonstrated that a computational biomarker can predict treatment outcomes in early-stage triple-negative breast cancer (TNBC) using pre-treatment biopsy images alone. The study, published in the Journal of the National Cancer Institute, evaluated 4D Path’s Q-Plasia OncoReader (QPOR™) platform, which applies statistical physics and tumor biology principles to digitized hematoxylin and eosin (H&E) slides.
The platform’s predictive model does not rely on clinical or molecular data. Instead, it assesses tumor immune response and cell-cycle activity directly from routine biopsy slides. This approach enables early prediction of chemotherapy response and may inform future applications in chemoimmunotherapy.
Study Design and Findings
The multi-institutional study included researchers from Dana-Farber Cancer Institute, Harvard Medical School, Brigham and Women’s Hospital, and 4D Path Inc. Investigators applied QPOR™ to pre-treatment core biopsies to evaluate tumor-infiltrating lymphocytes (TILs) and computational immune–cell-cycle biomarkers (CmbI), alongside independent visual assessments.
Key findings include:
- Paclitaxel Arm Prediction: CmbI predicted residual cancer burden (RCB 0/1) with an odds ratio of 9.17 (p=0.009; AUC 0.74) using H&E images alone.
- Immune Infiltration Correlation: Both visual and computational assessments correlated with treatment response.
- BRCA-Proficient Cohort: CmbI and visual TILs were associated with response overall, with predictive signals observed primarily in the paclitaxel arm.
The QPOR™ platform computes CmbI by integrating tumor proliferation, immune spatial heterogeneity, and G1/S cell-cycle deregulation signatures. Similar predictive performance was observed in TBCRC 031, which studied BRCA-mutated, HER2-negative breast cancer.
Implications for Clinical Practice
The study suggests that computational biomarkers derived from standard histology may complement traditional pathology and support treatment selection. The QPOR™ platform offers a reproducible, deterministic method that avoids observer variability and machine-learning bias. Its reliance on H&E images positions it as a scalable and interpretable alternative to conventional AI models.
Researchers note that this approach may assist in therapy selection, trial design, and early treatment adjustment strategies. The platform’s potential generalizability across tumor types is under further investigation.
For full details, refer to the article titled “Prognostic value of visually and computationally-assessed tumor-infiltrating lymphocytes in early-stage triple-negative breast cancer (TBCRC-030)” in the Journal of the National Cancer Institute.