The partnership represents a new model of AI medical billing and revenue cycle management powered by Clinical Language Understanding (CLU)
QueueLogix, a HealthChannels company, announces a new partnership with Nym Health, the forerunner in computational linguistics and autonomous clinical coding. The groundbreaking partnership pairs care team assistants (CTAs) – an evolution of the medical scribe – with a combination of QueueLogix and Nym software at the point of care to reduce coding and billing times, improve revenue cycles, enable patient engagement and increase compliance.
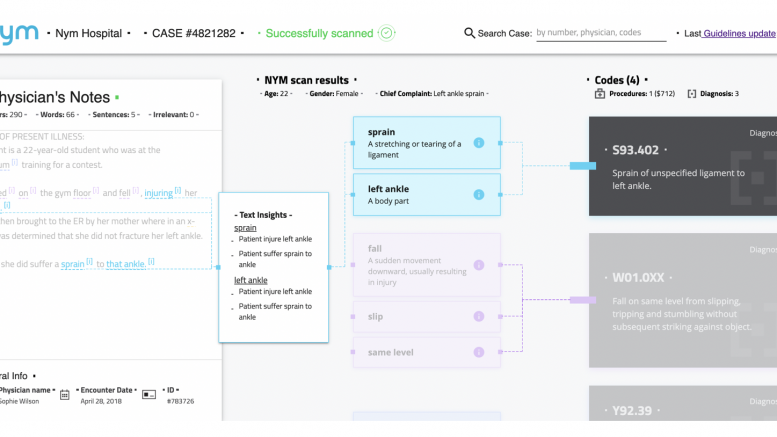
As CTAs document the patient encounter, Nym AI automatically identifies inconsistencies in clinical notes and assigns only the most accurate codes, in real-time. For charts it does not fully understand, the chart is flagged for scribes to resolve or placed in the coders’ queue for further action. The result is comprehensive coding without front and back-office siloes.
In addition, the partnership with Nym further refines the QueueLogix billing and coding solutions with a real-time audit dashboard. As the clinical codes are generated, the Nym audit-trail view provides an explanation for its rationale, giving CTAs and providers the opportunity to review codes for compliance and correct any documentation issues in real-time. With CTAs working in tandem via the QueueLogix LiveSuite workflow solution, and augmented by Nym AI capabilities, health systems are able to dramatically increase their RCM efficiencies and outcomes.
“The partnership with Nym and QueueLogix offers administrators a patient-centric solution to speed the cadence and quality of the coding and billing process,” says President of QueueLogix, Douglas Ingram. “We are excited about the synergy between the two companies, strengthened by HealthChannels’ ability to redeploy labor where it matters most. Typical solutions in the market unnecessarily place burdens on providers and back-office personnel. With our solution, CTAs are able to interface with technology in a real-time manner to drive efficiency in coding and billing outcomes, while also improving the patient experience.”
“As high deductible plans increase threefold, more of the healthcare costs have become the burden of the patient,” continues Ingram. “Retooling billing work-flows and determining coding at the point of care in real time with Nym allows us to engage the patient in a more meaningful and impactful interaction. This is the next evolution of our LiveCode offering and we are very excited to bring it to the market.”
With repeatable and detailed coding, the QueueLogix–Nym solution consistently produces a more accurate medical chart for increased reimbursement. The QueueLogix LiveSuite platform deployed alongside the client’s EMR, utilizing Nym’s Clinical Language Understanding (CLU) capabilities, gives stakeholders more accurate and actionable reimbursement data faster than any solution available today. Across care settings, administrators and stakeholders will also benefit from the combined offering’s advanced data analytics capabilities to track coding trends and performance over time to inform RCM strategies.
“We are pleased that HealthChannels shares our recognition of the need for autonomous coding,” said Amihai Neiderman, CEO and co-founder of Nym. “Our unique approach to language understanding successfully uses computational linguistics in the medical domain, offering fast, accurate and auditable coding. Nym’s medical knowledge layer, combined with the QueueLogix LiveSuite platform and HealthChannels’ base of 25,000+ professional CTAs and scribes, serves as a new best practice, freeing up clinicians to focus on patients, and offering patients real-time access to their bills.”
The technology will be available to current care team assistant and scribe clients and health systems looking to recoup revenue previously lost due to billing cycle inefficiencies.