by Cureatr’s Kent Hiller, VP Market Development and Dana Fieni, Director of Sales
If you are reading this, it means you survived Year 1 of the DSRIP program in New York. Congratulations! Hopefully you celebrated the New Year on April 1 like we did – with a cup of coffee and a morning dose of the CMS Innovation Center.
Year 1
Across the state, DSRIP Year 1 saw Performing Providers Systems (PPS) receive initial patient attributions, assess network capabilities, strengthen organizational structures, and begin the long process of workflow engineering along with vendor partner evaluation. Also, (and this may not sound surprising) getting organizations of various sizes to coordinate care under one PPS umbrella is complicated. This is because smaller providers may have limited IT departments or budgets, and challenges or kinks in technology will affect each PPS organization differently.
Everyone is running their own EMR software and utilizing disparate IT infrastructure. Because of this, we see an appetite for new technologies which are easy to implement, have lower cost points, and include mobile delivery mechanisms that will create a level playing field across the industry as providers of all shapes and sizes focus on care coordination and participate in payment reform programs.
The innovation also taking place is in the area of episodic patient data sharing. PPS’ are connecting various levels of care to align and coordinate the flow of patients and patients’ data throughout care episodes. This means connecting Health Homes, PCP and specialist clinics, Home and Community Based Services (HCBS), Post-Acute Care, and Acute Care Hospitals into operational project-focused care and data channels. This immense task is being approached iteratively, combining small impactful steps to aggregate greater networks. Each PPS confronts unique challenges to connecting its care continuum, though each continues to adjust organizational structures to guide practices toward project and program goals. On the immediate horizon is the deployment of innovative healthcare IT solutions to cement, stabilize and support these fledgling care networks.
In September 2015, New York State Medicaid Director Jason Helgerson, delivered helpful mid-year updates, available here. According to Jason, midway through the first full year of DSRIP in New York, PPS organizations were transitioning from planning to implementation. He raised a few reminders, which bear repeating, including:
- That teams from KPMG are making site visits and sharing best practices. Jason encouraged PPS to utilize KPMG resources as needed.
- The Medicaid Accelerated eXchange, or MAX series, launched in October with the first pilots and are currently in the “PDSA – Plan Do Study Act” phase, which is consulting-speak for: design, implement, review and improve. The pilot period ends in September 2016, so we’ll be excited to hear how things went.
Year 2
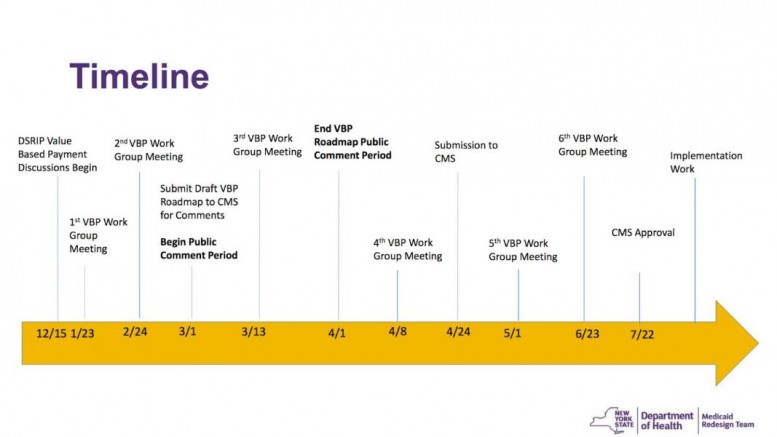
DSRIP Year 2 will culminate in the transitions to Pay for Performance (P4P), as trending metrics will begin to influence incentive payments. The MAPP dashboards will continue to evolve, assessor evaluations of quarterly reports will gain consistency, and the State’s overall Value Based Payment Roadmap will gain clarity. (see image for Timeline)
To help the public understand what “Value Based Payments” are all about, the New York State Department of Health published a helpful two minute video in November. It hits on the right key points and articulates the end goal for many of these reform programs.
We look forward to having a few opportunities in 2016 to get out from behind our computer screens and gather in person to share learnings and hear results. Mark your calendar for May 3 for the Downstate symposium, May 17 for the Upstate symposium, and September 20 – 22 for the Statewide symposium.
Year 2 will move quickly and it’s important to keep an eye on the horizon. Any structural changes must be done and implemented by the start of Year 3, April 1, 2017. This is when performance really starts to count because payments will be linked to outcomes. PPS organizations looking for ways to improve care coordination and communication which will reduce avoidable hospitalizations can consider utilizing Cureatr’s New York Network of Care Transition Notifications. This network provides real-time, actionable alerts anytime an attributed patient has a care event in the region.
What do you think the biggest achievement will be in DSRIP Year 2? Who will the big winners be? Will there be any losers?
Send your thoughts to info@cureatr.com or post on Cureatr’s Facebook page.